A Lifeline Between Appointments: Supporting Frequent Attenders in Primary Care
For many people living with complex or long-term health conditions, a GP’s office can feel like the only safe harbour in a storm, a place where they are truly seen and heard. Research suggests that the top 10% of consulting patients account for around 40% of all GP appointments in the UK (Kontopantelis et al., 2021), a reminder that a relatively small group of frequent attenders can drive much of the system’s workload. More importantly, it reflects a broader gap in how ongoing support and self-management are embedded within routine care.
Bridging that gap requires new ways of connecting care beyond the clinic. Digital health tools can play an important role by offering people timely support, motivation, and guidance between appointments. Used well, they can help individuals build confidence in managing their own health, strengthen continuity of care, and ultimately reduce pressure on frontline services.
This analysis focuses on data collected from over 3,700 Holly Health users identified as frequent attenders (defined as individuals who reported three or more GP visits in the eight weeks before joining Holly Health), who completed onboarding questions. We then analysed data from users who had low-to-medium scores at baseline for each measurement area (defined as selecting an option corresponding to a score of 1 to 3, out of 5 on a Likert scale) and who responded to our follow-up surveys (n = 327).
Baseline Health Profile: A Complex Clinical Picture
At baseline, this cohort (3,700 people) presented with several prevalent and often co-existing health conditions, highlighting opportunities to strengthen wellbeing and self-management support.
Living with Profound Fatigue: A significant, 68.3%, of individuals reported feeling tired most days. This level of fatigue may contribute to a barrier to engaging in positive health behaviours. For context, this is considerably higher than the 53% reported by the average Holly Health user.
Elevated Stress Levels: Over half of the cohort (50.6%) rated their stress in the last two weeks as "Very High" or "High”. This indicates a state of chronic strain that is much more prevalent than in the general Holly Health user population, where the figure is 39.4%.
High Prevalence of Mental Health Conditions: Nearly half of the individuals were living with anxiety (46.9%), and a large portion reported depression (41.8%). These conditions can often underpin and exacerbate other physical health issues.
Daily Life More Heavily Impacted: The burden of these conditions was tangible. Nearly a third of users (32%) stated that their ability to carry out their usual daily activities was heavily affected, almost double the 16.3% reported by the average user.
.png)
Health Outcomes: Measurable Improvements After 8 Weeks
After 8 weeks of using Holly Health, frequent attender users showed statistically significant improvements across all reported measures (p < .001). These findings are based on data from 327 participants who completed both onboarding and 8-week follow-up surveys. The results demonstrate a clear shift towards substantial progress across multiple wellbeing and self-management measures, with percentages reported relative to baseline.
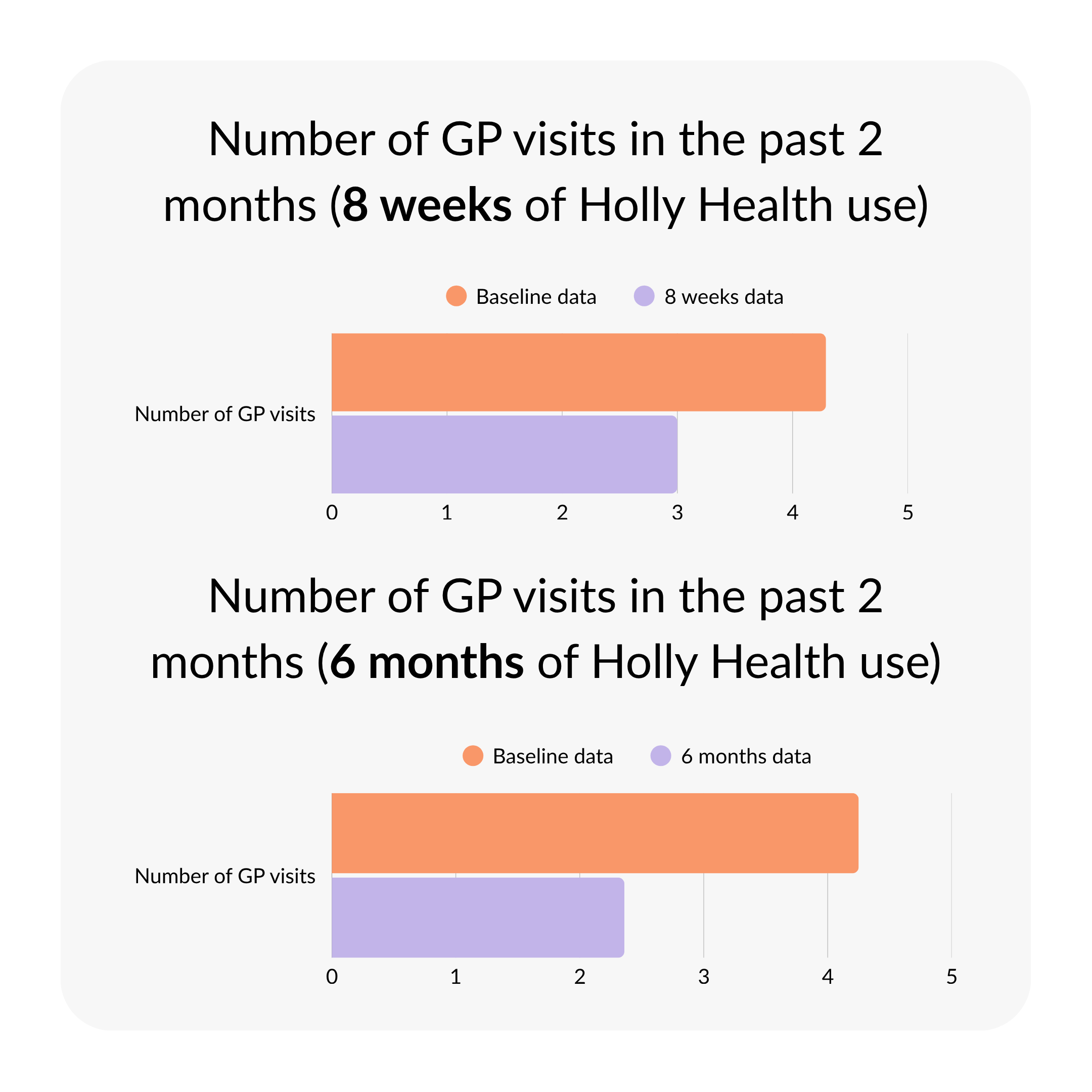
Reduced Primary Care Attendance (30% Decrease in GP Visits): The most notable outcome was a reduction in reliance on primary care services. Users' average GP visits decreased from 4.29 to 3.00 over the eight-week period. This translates to a potential reduction of 8.4 appointments per person, per year, freeing up vital NHS resources.
This positive pattern continued over time. Follow-up data from 86 users at 6 months revealed a 44% sustained reduction in GP appointments, equivalent to around 12 fewer appointments per person annually if maintained.
After one year, data from 69 users showed that the reduction in GP appointments was largely maintained, with an overall 36% decrease compared with baseline levels.
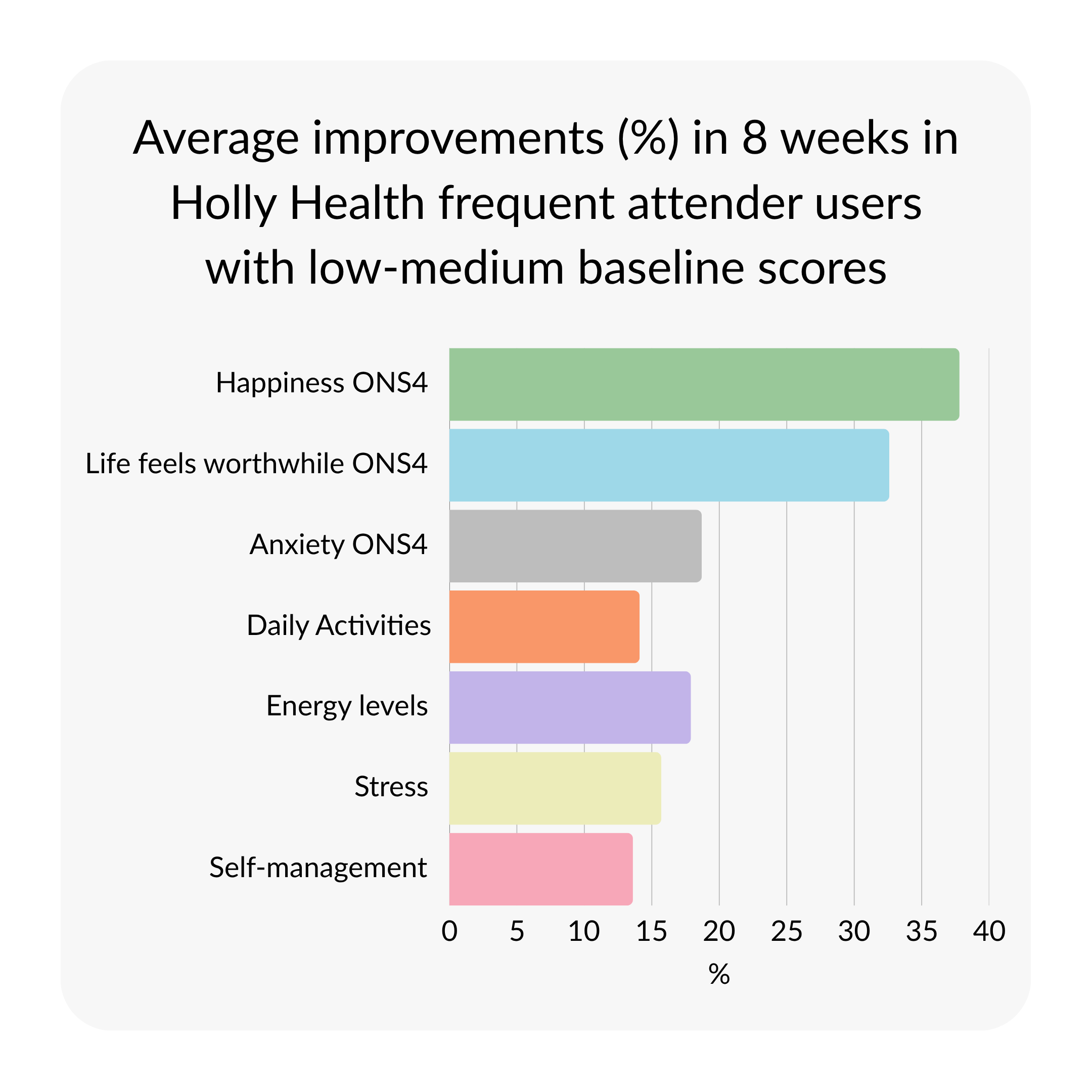
Significant Gains in Personal Wellbeing: Building on the high baseline prevalence of anxiety and depression, users reported an average 31.3% increase across all four ONS4 measures of personal wellbeing. The most pronounced gains were a 37.8% increase in happiness and a 32.6% increase in feeling that life is worthwhile.
Effective Anxiety Reduction: Average ONS4 Anxiety scores decreased by 18.7%, from 7.23 to 5.88 (where a lower score indicates better outcomes). This reflects a meaningful reduction in self-reported anxiety, which affected 46.9% of the cohort at baseline.
Improved Daily Functioning: At baseline, 32% of users reported that their daily lives were heavily impacted by health challenges. After engaging with Holly Health, the cohort reported a 14.1% gain in their ability to carry out usual daily activities, a key indicator of enhanced quality of life.
Higher Energy and Lower Stress: Participants made notable progress in addressing baseline fatigue and stress. Energy levels increased by 17.9%, while self-reported stress decreased by 15.7%, reflecting greater resilience and overall wellbeing.
Increased Self-Management: As users gained practical tools and confidence to manage their health, their self-reported ability to self-manage increased by 13.6%.
This community also demonstrated meaningful progress in other lifestyle areas, including a 30.3% increase in moderate exercise, showing a broader shift toward sustainable behaviour change.
Habits Supporting Mental and Emotional Wellbeing
The habits this group chose to develop first reveal much about their needs and motivations. Unlike other user groups who often begin with physical health goals, these participants prioritised habits such as positive body affirmation, meditation, and calm thinking. Alongside these, they also selected familiar wellbeing foundations such as stretching, walking, and drinking water, habits that appear consistently across Holly Health cohorts. This pattern highlights a balanced approach, combining emotional regulation with practical steps toward better everyday wellbeing.
"It Has Made Me Feel That Someone Cares"
The qualitative feedback from this cohort provides valuable insight into the experiences driving these changes. Users consistently highlighted a shift from feeling overwhelmed to feeling more supported and empowered.
The feeling of having a consistent, non-judgemental companion was often mentioned as transformative. As one person shared: "I find it very helpful. It has made me feel that someone cares." Another user reflected on a growing sense of self-efficacy: "I think the app is very useful. It has helped me to try and help myself where I can."
Together, these reflections suggest that for people living with complex health needs, meaningful progress is supported not only through clinical appointments, but also through what happens between them. Consistent encouragement, compassion, and small, achievable actions can help people sustain the benefits of care and build confidence in managing their health day to day. As one user advised others just beginning their journey:
"Don't think twice about it. Give it a go. It helped me believe in myself again."
For our partners in the NHS and beyond, these findings offer valuable insight into how best to support patients with complex needs. The reduction in GP appointments is not only a sign of reduced demand but also an indication that users are experiencing better wellbeing and greater confidence in managing their health. Importantly, this change occurred alongside broad improvements across other areas of health, from daily functioning to mental resilience. Together, these outcomes point to stronger self-management and engagement with care, rather than withdrawal from it. By equipping patients with tools that build confidence and autonomy, we can help create a more collaborative, compassionate, and sustainable model of primary care that benefits both patients and the system as a whole.










.jpg)

