Data insights report from existing female users with problematic eating behaviours
Introduction
Binge Eating Disorder (BED) is a major but often overlooked public health issue, particularly among women. NICE estimates that the prevalence in women is 6x higher than in men in Europe. In the UK, 26% of women have obesity, and around 30% of individuals with obesity and weight loss goals exhibit symptoms of Binge Eating Disorder (BED), potentially affecting over three million women. Binge eating episodes can escalate to BED, which costs the NHS over £3.5 billion annually. Early intervention of problematic eating behaviours is essential for reducing BED prevalence and healthcare costs.
One of the key drivers of BED is diet- and calorie-restriction-focused weight loss methods, which remain common despite often poor long-term outcomes. Restrictive dieting can unintentionally contribute to cycles of restriction and binge eating. In contrast, evidence-based approaches such as mindfulness and intuitive eating offer more sustainable solutions (Friedel et al., 2015; Mercado et al., 2021). These methods help individuals reconnect with natural hunger and fullness cues, reduce emotional eating, and improve self-regulation. When delivered digitally, they have the potential to reach large numbers of people at low cost and with high scalability.
This insights report is part of an SBRI-funded project that seeks to significantly increase women’s access to support for problematic eating behaviours by incorporating a mindfulness and intuitive eating coaching journey into HollyHealth. Holly Health is a fully digital, personalised health coaching app that supports users to make sustainable behaviour changes across physical and mental health. With 70% of its users identifying as female and 56% reporting problematic eating behaviours, Holly Health is well-positioned to address this critical gap in care.
Methods
Female users who reported a problematic relationship with food during the onboarding process were included in this analysis. Users were invited to complete a ‘behavioural health check’ through the Holly Health app at four time points: onboarding (prior to using the service), and at 8 weeks, 6 months, and 12 months following engagement.
The ‘behavioural health check’ consists of a set of questions aimed at assessing four main areas that are mental health, physical health, relationship with food and sleep. The same questions were used at each time point to allow for comparison over time and to inform personalised coaching and recommendations within the app.
For this report, we analysed data from 987 female users who, during onboarding, rated their relationship with food as low to medium on a 5-point Likert scale (defined as selecting an option corresponding to a score of 1 to 3). The same Likert-style question was used in follow-up surveys, allowing for direct comparison of responses over time.
Insights
Demographics
The most prevalent age ranges were 55–56 years (29%) and 45–54 years (27.4%).
Goals
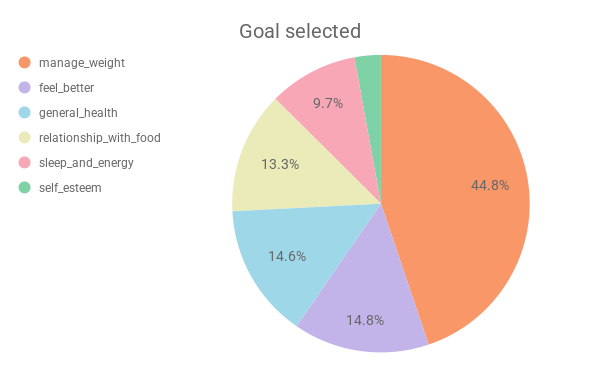
Nearly half of the responders (45%) selected weight management as their main goal when joining Holly Health, highlighting it as a key motivation for engagement. Others were more focused on overall wellbeing, with goals like feeling better (15%), improving general health (15%), and building a healthier relationship with food (13%). A smaller number of users chose goals like boosting sleep and energy (10%) or improving self-esteem (3%). Overall, it’s clear that while weight management is a key motivation, many users are also looking for broader support with their physical and emotional health.
Medical conditions
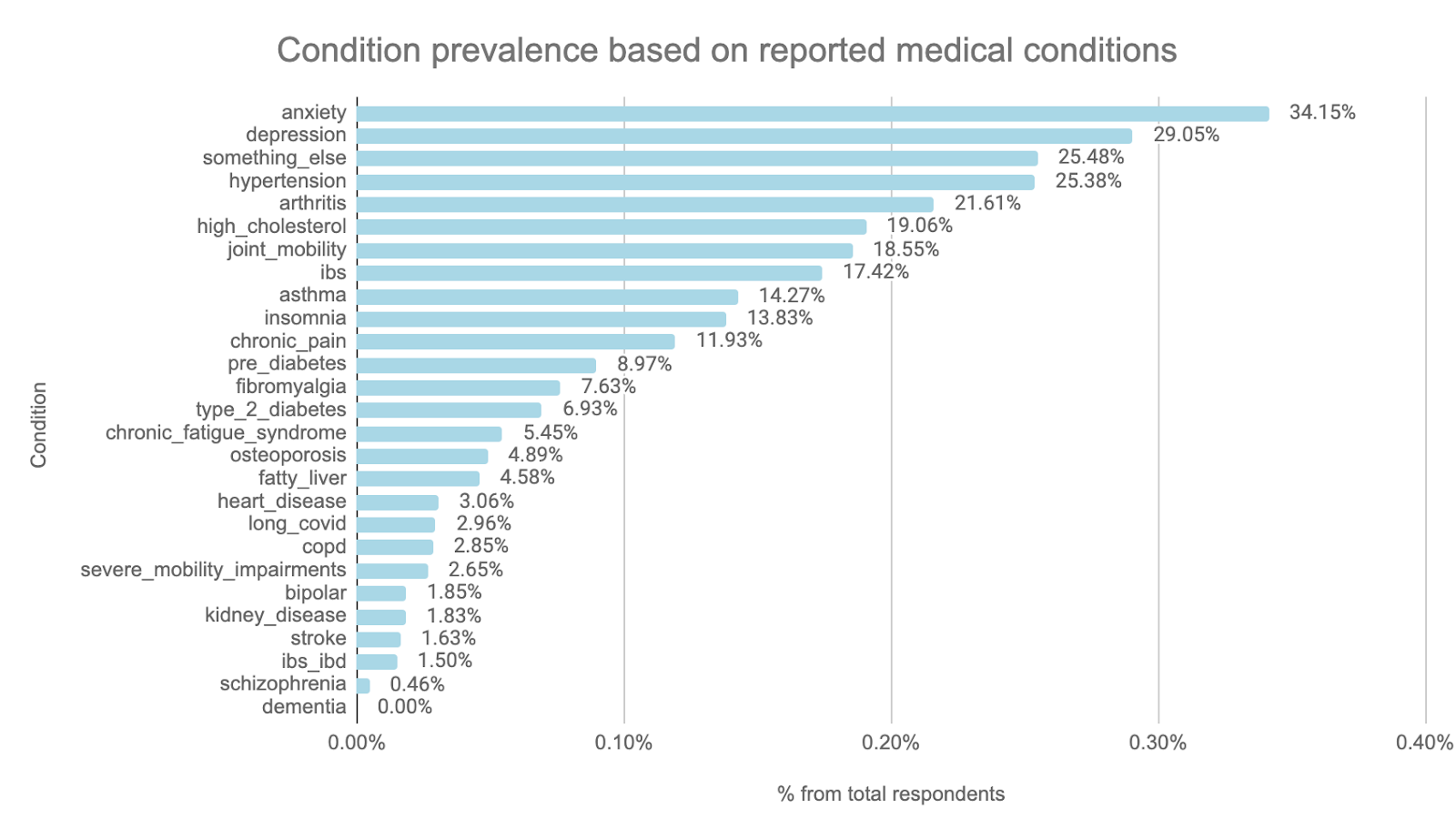
Among the 981 users who disclosed medical conditions at onboarding, the most frequently reported were anxiety (34%) and depression (29%), followed by physical health conditions such as hypertension (25%), arthritis (22%), and high cholesterol (19%). Other commonly reported conditions included joint mobility issues (19%), IBS (17%), and chronic pain (12%). The high reporting rates of both mental and physical health conditions highlight the diverse and often complex health backgrounds of users who self-reported a low relationship with food. This suggests that these users are also managing co-existing health challenges that may shape their day-to-day wellbeing and routines around food.
This aligns with national trends: 1 in 4 adults in England experience a mental health problem each year (Mind), and around 30–46% of people with a long-term physical condition also experience a mental health condition. Conversely, 46% of those with a mental health condition have at least one long-term physical health issue (Cambridgeshire Insight, 2024). These figures reflect the extent to which mental and physical health often co-exist in the general UK population and help contextualise the high rates observed in this group.
Eight-week outcomes: Improvements in the relationship with food and other health outcomes
Eating behaviours
After eight weeks of using the Holly Health app, there was a statistically significant improvement in users’ relationship with food scores (p < 0.01). Among the 782 users who responded, those with low to medium baseline scores showed an average improvement of 38% compared to their baseline scores, and an absolute change of 13% on the full scoring scale, indicating meaningful early progress. One person reflected:
“Really like the app and do think I am benefiting. Find it encouraging and am taking time to think how I feel before eating - often eat without thought when stressed and tired. Habits are thought-provoking and achievable.“
Other outcomes related to eating behaviours also showed statistically significant improvements at eight weeks. Among 439 respondents, fruit and vegetable intake improved by 16% from baseline and 8% in absolute terms, equivalent to an average of 1–2 additional portions per week. Similarly, 170 users improved their dinner-time habits by 23% from baseline and 12% in absolute terms, specifically around leaving more time between eating and going to bed. These changes suggest positive shifts in daily routines that support healthier eating patterns.
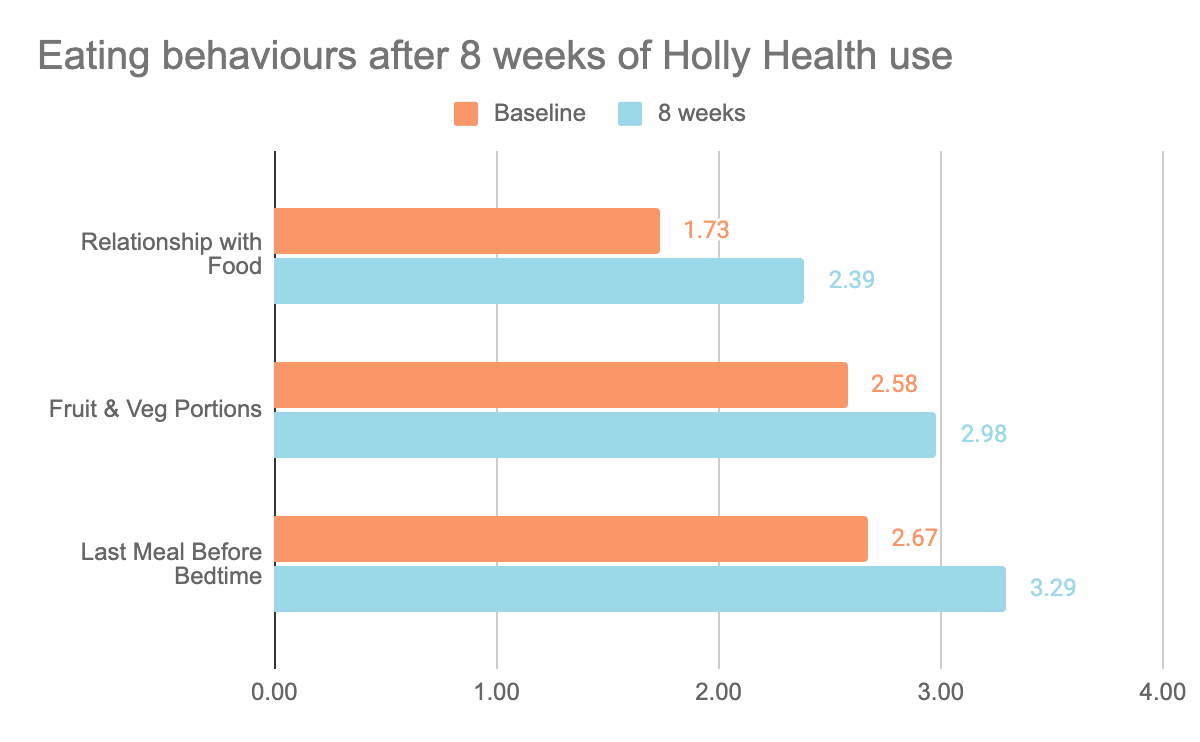
Eating behaviours score changes (%):
- Relationship with food: 13%**
- Fruit & Veg Portions: 8%**
- Last Meal Before Bedtime: 12%**
**p<0.001
Personal wellbeing
Statistically significant improvements were seen across all four areas of personal wellbeing at eight weeks, as measured by the ONS-4, a validated tool from the Office for National Statistics. On average, happiness increased by 33% compared to baseline, with an absolute gain of 11% on the full scoring scale. Anxiety decreased by 21%, corresponding to an absolute reduction of 15%. Life satisfaction and the sense of life being worthwhile both improved by 27% relative to baseline, with an absolute change of 10% in each case. These changes are especially relevant given that during onboarding, 34% of female users reported anxiety and 29% reported depression as existing medical conditions. The number of respondents for these outcomes ranged from 292 to 497.
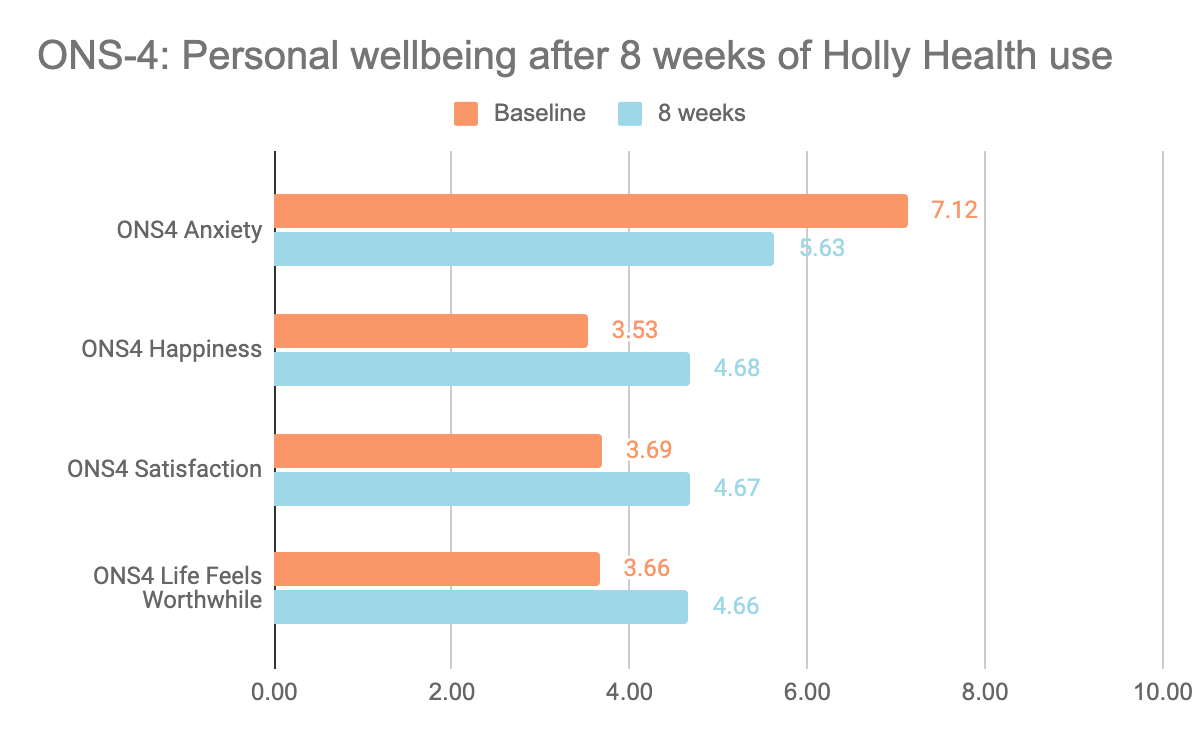
ONS-4 score changes (%):
- ONS4 Anxiety: -15%**
- ONS4 Happiness: 11%**
- ONS4 Satisfactions: 10%**
- ONS4 Life feels worthwhile: 10%**
**p<0.001
Other health outcomes
Alongside improvements in eating behaviours, users also reported statistically significant improvements in physical wellbeing, including better sleep, increased energy, and higher levels of exercise at 8 weeks. On average, sleep habits improved by 8% from baseline, with an absolute gain of 4%, and energy levels rose by 18%, reflecting an absolute increase of 8%. Positive changes were also observed in physical activity: moderate exercise (e.g., brisk walking, running, cycling) increased by 29%, with an absolute shift of 12%; flexibility and strength exercises rose by 21% and 16%, with absolute gains of 7% and 4%, respectively. These outcomes indicate positive changes in physical wellbeing and are based on self-reported data from between 524 and 749 users. One user’s comment reflects this:
“Holly has helped me to build good habits with food and exercise. Even small improvements have a big impact on your overall health.”
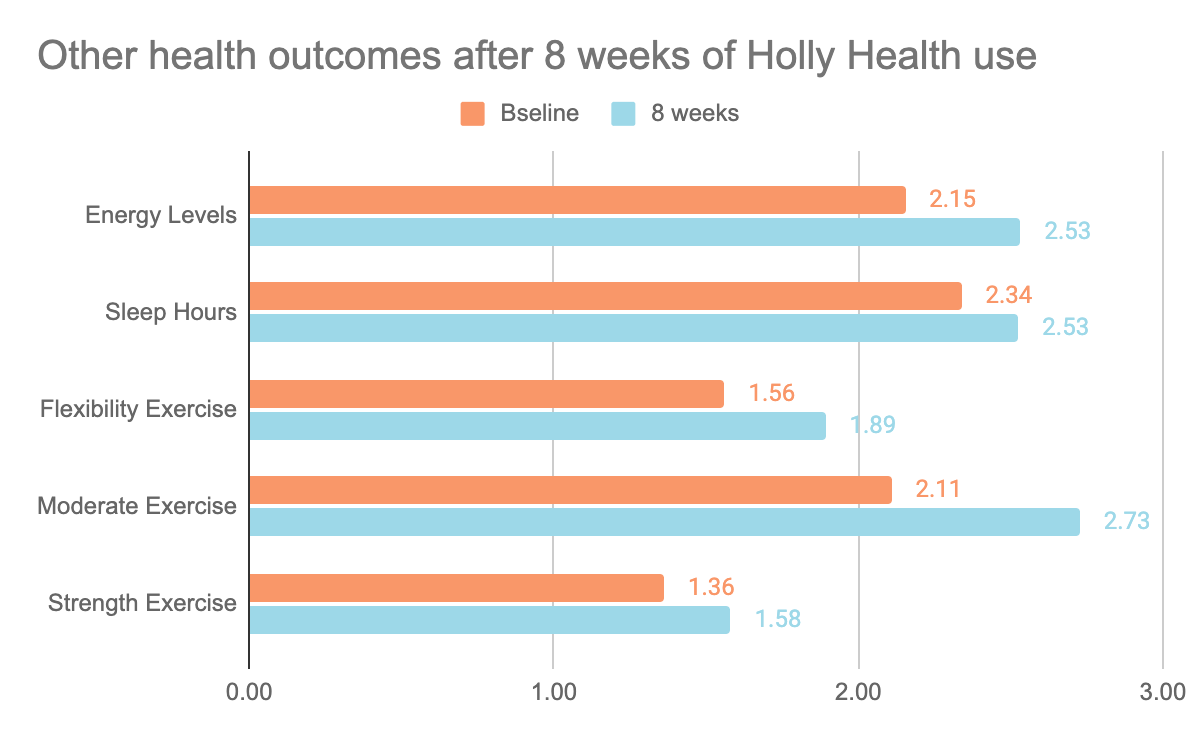
Health score changes (%):
- Energy levels: 8%**
- Sleep: 4%**
- Flexibility Exercise: 7%**
- Moderate Exercise: 12%**
- Strength Exercise: 4%**
**p<0.001
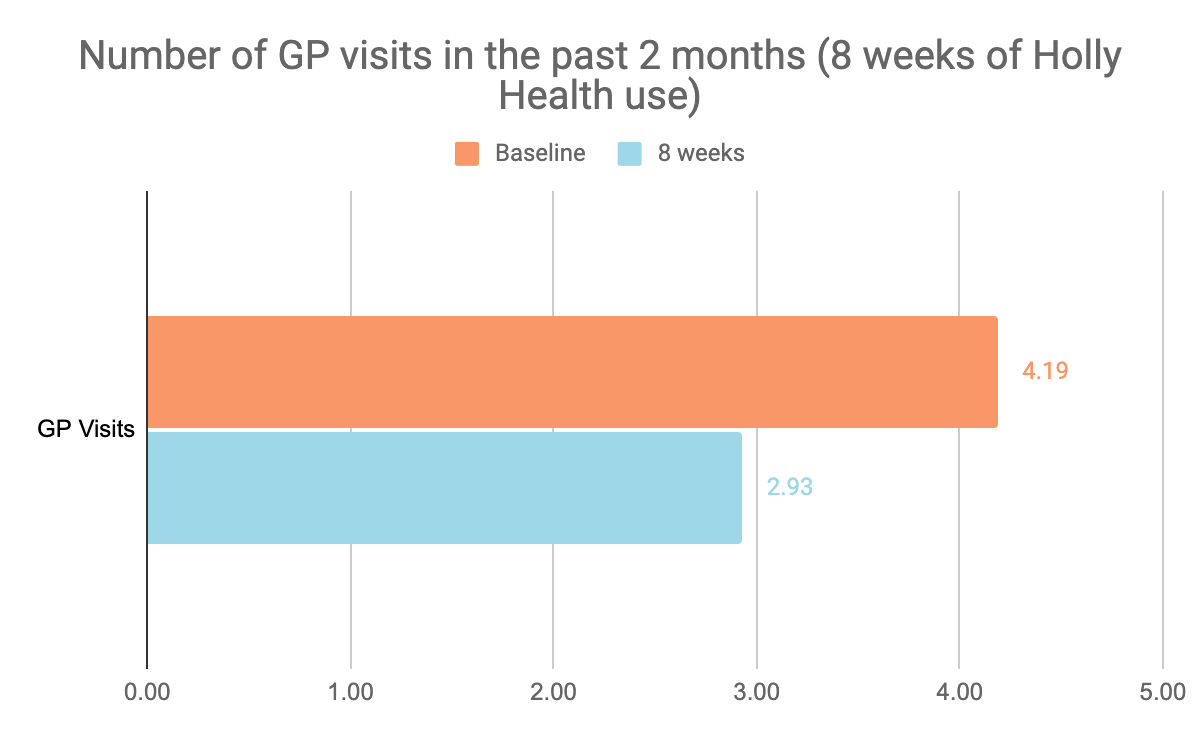
Self-management
In addition to improvements in wellbeing and behaviour, Holly Health was associated with a reduction in demand for primary care services. The number of GP visits decreased by 30% after eight weeks of Holly Health use, compared to the baseline reported at onboarding. This could suggest that users may be managing aspects of their health more independently after using the app. One respondent explained:
“Having greater awareness of my health through the app has helped me take control of my health. Holly Health makes me think about my mood, stress levels, and at the moment food satisfaction.“
Longer-term outcomes: Continued improvement in the relationship with food
Data from the ‘behavioural health check’ follow-up at six and twelve months shows that positive changes in relationship with food were sustained over time. At six months, there was a statistically significant average improvement of 55% compared to baseline, with an absolute gain of 17%, based on responses from 266 users. At the twelve-month mark, the average improvement reached 37%, with an absolute change of 13%, based on data from 206 users. These results suggest continued progress among users who remained engaged with Holly Health. One participant recounted:
“The tips and information provided are really useful in helping me understand more about my relationship with food.”
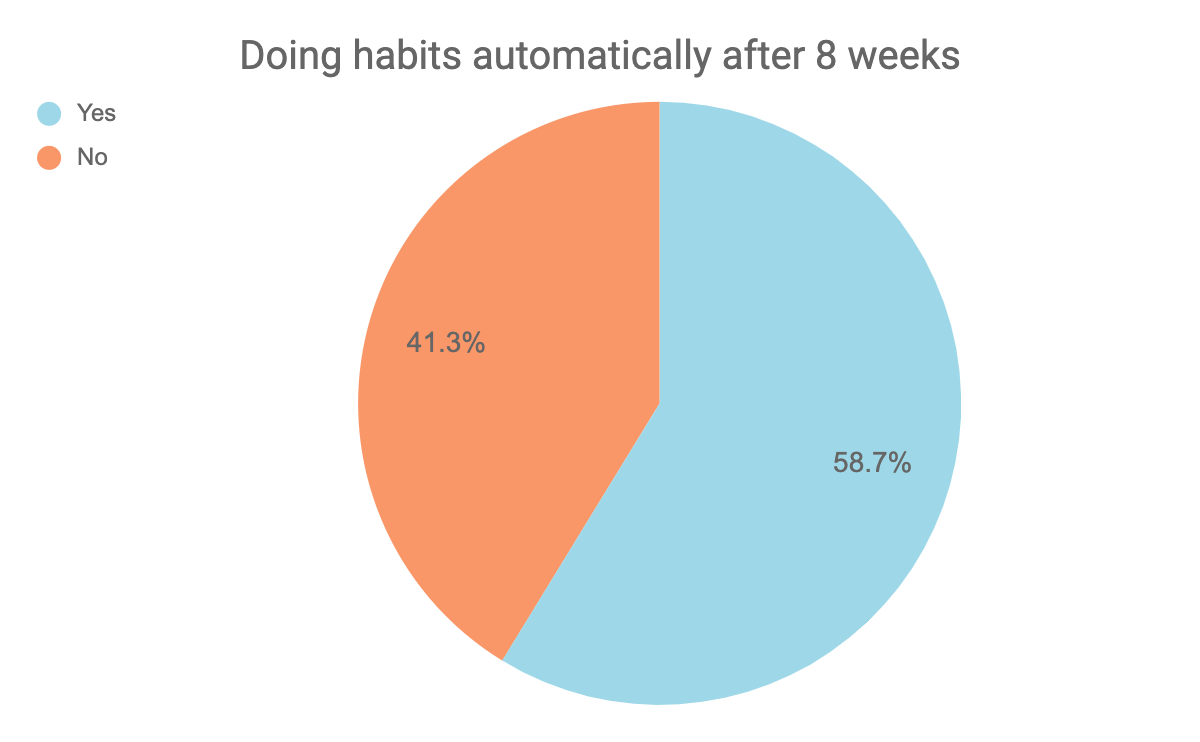
Engagement metrics
On average, responders started four new individual health habits, with a median of three per person. This refers to the number of distinct habits selected in the app, such as “practice food satisfaction” or “spend time outdoors.” In terms of habit completions (the number of times users actively marked a habit as done), the mean was 106, while the median was 10. This indicates a wide range in engagement, with many users completing a smaller number of habits, and a smaller group contributing to a higher average through more frequent use. Importantly, 59% of users reported that they were completing their healthy habits automatically as part of their normal routine by the end of the eight-week period. This may partly explain lower manual tracking, as behaviours became integrated into daily life and were no longer actively marked in the app. Users commented on their experience:
“The Holly health app has been a great help in establishing new habits. It's empowered me to know that I can make small changes to my diet and routine that will quickly become permanent.”
“The habits I do regularly are pausing during eating to check my hunger levels and taking time to check in on my emotions.”
Link between habit completion and relationship with food scores
A Spearman’s rank correlation was conducted to explore the relationship between habit completion and relationship with food scores across three different points. While habit completions were not time-specific, the analysis provides insight into how overall engagement may relate to perceived improvements in eating behaviours over time. At the first follow-up (eight weeks), the correlation was not statistically significant, suggesting no clear association at that stage, rs(782) = .065, p = .069. However, at both the six-month and twelve-month follow-ups, statistically significant positive correlations were found, rs(266) = .125, p = .042, rs(206) = .213, p = .002, respectively. This indicates that users who completed more habits over time tended to report a better relationship with food, particularly at the six- and twelve-month follow-ups.
Conclusion and next steps
These early findings highlight Holly Health’s strong potential to improve users’ relationship with food. Alongside this core outcome, users also reported positive changes in personal wellbeing, energy levels, physical activity, and sleep, indicating wider benefits to overall wellbeing. While these trends are highly encouraging, there remains room to strengthen the impact even further.
Holly Health’s small habits approach aims to support sustainable behaviour change. This model was reflected in the data, with correlation analysis showing a significant positive association between total habit completion and relationship with food scores at the six- and twelve-month time points. While habit completion clearly plays a key role, there is an opportunity to improve outcomes through evidence-based features specifically designed to support users experiencing binge eating behaviours.
This report focused on individuals who reported a low relationship with food at onboarding, a group likely to include some users with unrecognised or sub-clinical binge eating behaviours. To enhance support, while we used a broad relationship with food measure in this phase, future work should focus more directly on identifying and supporting users with binge eating patterns. This would include refining onboarding questions and tailoring the coaching journey to better meet the needs of this underserved group.
Overall, the overwhelmingly positive outcomes in this cohort highlight the potential of Holly Health as a digital health tool to support people experiencing problematic eating, such as loss of control around eating. It offers a scalable and cost-effective approach that can lessen the burden on both individuals and the healthcare system.
Looking ahead, Holly Health is developing several new features aimed at deepening user engagement and further improving outcomes across measured areas. These include the Insight Path, which guides users through personalised journeys based on their goals, early designs for a Food and Mood Diary, which aims to support awareness of eating habits and a community feature for insights sharing and education to help. As these features are rolled out, we expect continued improvements across key measurement areas, particularly among users seeking to improve their relationship with food.












