Seven Points Lower: The Power of Small Habits in Hypertension Management
High blood pressure, or hypertension, is one of the most common long-term health conditions. It is estimated that it affects around one in three adults in the UK, yet many remain unaware that they have it (British Heart Foundation, 2025). Because the condition rarely causes obvious symptoms, it has earned the description of the ‘silent killer’. When left unmanaged, hypertension significantly increases the risk of cardiovascular disease, including heart attacks and strokes, which remain among the leading causes of death nationwide (NHS, 2024).
While genetics play a role, the risk of developing hypertension is largely shaped by our environmental and daily habits (Carey et al., 2018). NHS guidance is clear that lifestyle change should be the first line of treatment for most people with high blood pressure. Research shows that physical activity, healthier eating, maintaining a healthy weight, improving sleep and managing stress can all play a powerful role in lowering blood pressure and reducing future risk (Charchar et al., 2024).
Yet knowing what to do is rarely the hardest part. For many people, the real challenge lies in turning advice into action, particularly when low energy, stress and long-established routines make change feel overwhelming. To understand what sustainable change looks like in practice, we analysed data from over 5,850 Holly Health users living with hypertension.
Baseline Health Profile
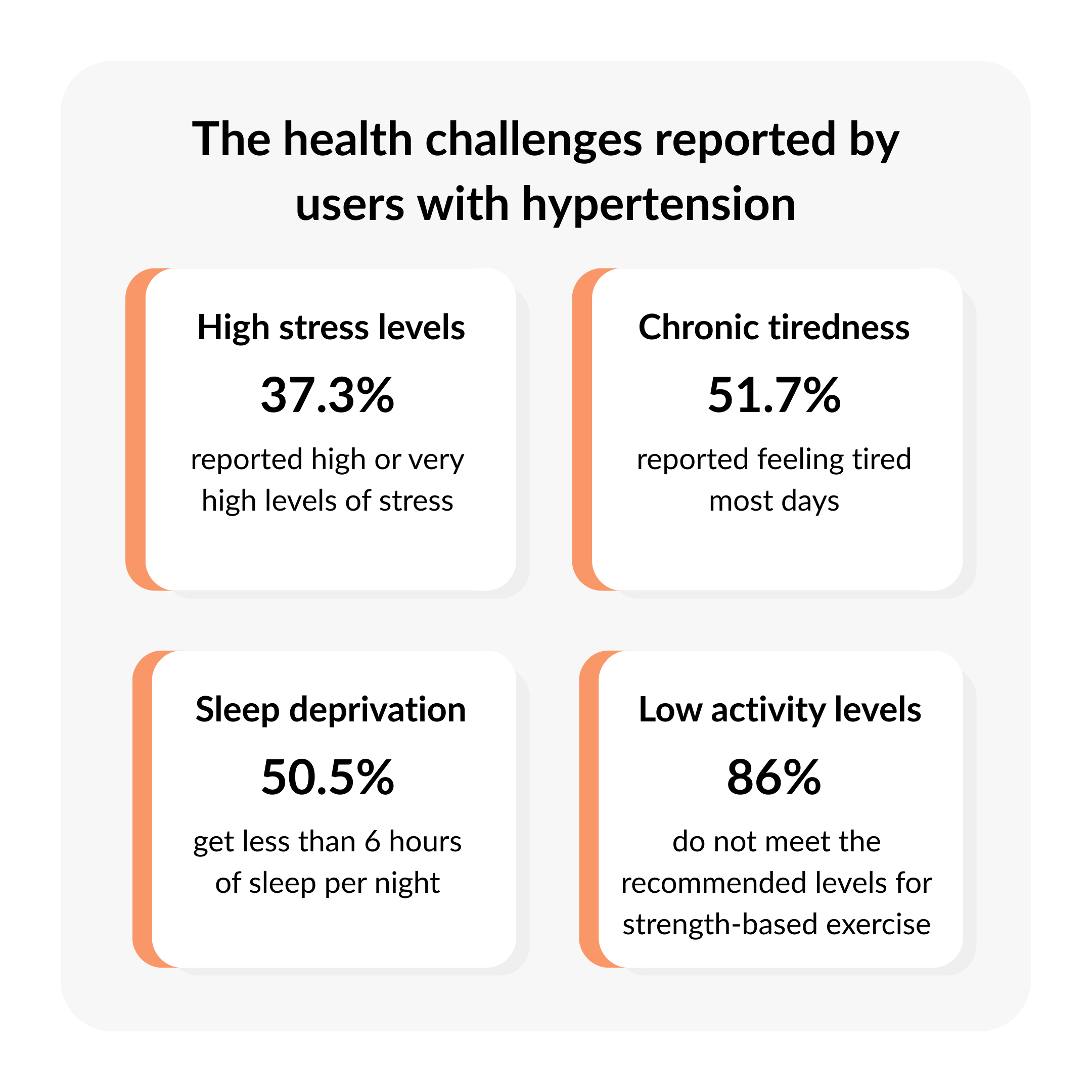
The onboarding data from this cohort (5,850 individuals who reported a diagnosis of hypertension) provided important context for understanding the barriers and opportunities for lifestyle-based hypertension management, revealing high levels of fatigue, stress, insufficient sleep and low physical activity across the group.
An Older, Higher Risk Population: More than 65% of users were aged 55 or over, an age group for whom effective blood pressure management is particularly important in reducing the risk of future cardiovascular events. In this age group, hypertension commonly coexists with other long-term conditions and age-related physiological changes, increasing the importance and potential complexity of lifestyle-based management approaches (NICE, 2023).
Weight Management as a Key Motivation: Almost half of users (45.6%) identified weight management as their primary goal. This is consistent with established evidence linking excess body weight with elevated blood pressure and increased cardiovascular risk, particularly in middle-aged and older adults (Lin et al., 2024). While this suggests awareness of the role of weight in hypertension management, it also points to the potential need for structured support to help individuals navigate dietary and lifestyle changes effectively.
The Hidden Burden of Stress: Nearly two in five users (37.3%) reported high or very high stress levels at baseline. Psychological stress and related psychosocial factors have been associated with elevated blood pressure and increased hypertension risk in observational and longitudinal studies (Marwaha et al., 2022). Although causality cannot be inferred from self-reported stress alone, these findings highlight stress as a relevant contextual factor within this population.
Energy, Sleep and Capacity for Change: Over half of the cohort reported feeling tired most days (51.7%), and 50.5% reported sleeping fewer than six hours per night. Insufficient sleep and persistent fatigue have been linked to reduced engagement in physical activity and other health-promoting behaviours, which may influence an individual’s capacity to initiate or maintain lifestyle changes (Itani et al., 2017).
Low Baseline Activity Levels: At baseline, 44% of users were below national guidelines for moderate physical activity, and 86% were not meeting recommended levels for strength-based exercise. These figures are notable given the high prevalence of fatigue and poor sleep reported within the cohort, factors which may limit engagement with physical activity.
Outcomes After 8 Weeks: Measurable Steps Forward
After eight weeks, we analysed user data to evaluate whether small, daily habit changes translated into measurable health improvements. In this analysis, we focus on data from users who had low-to-medium baseline scores across measurement areas (defined as selecting an option corresponding to a score of 1 to 3, out of 5 on a Likert scale) and who completed our follow-up surveys (n = 512).
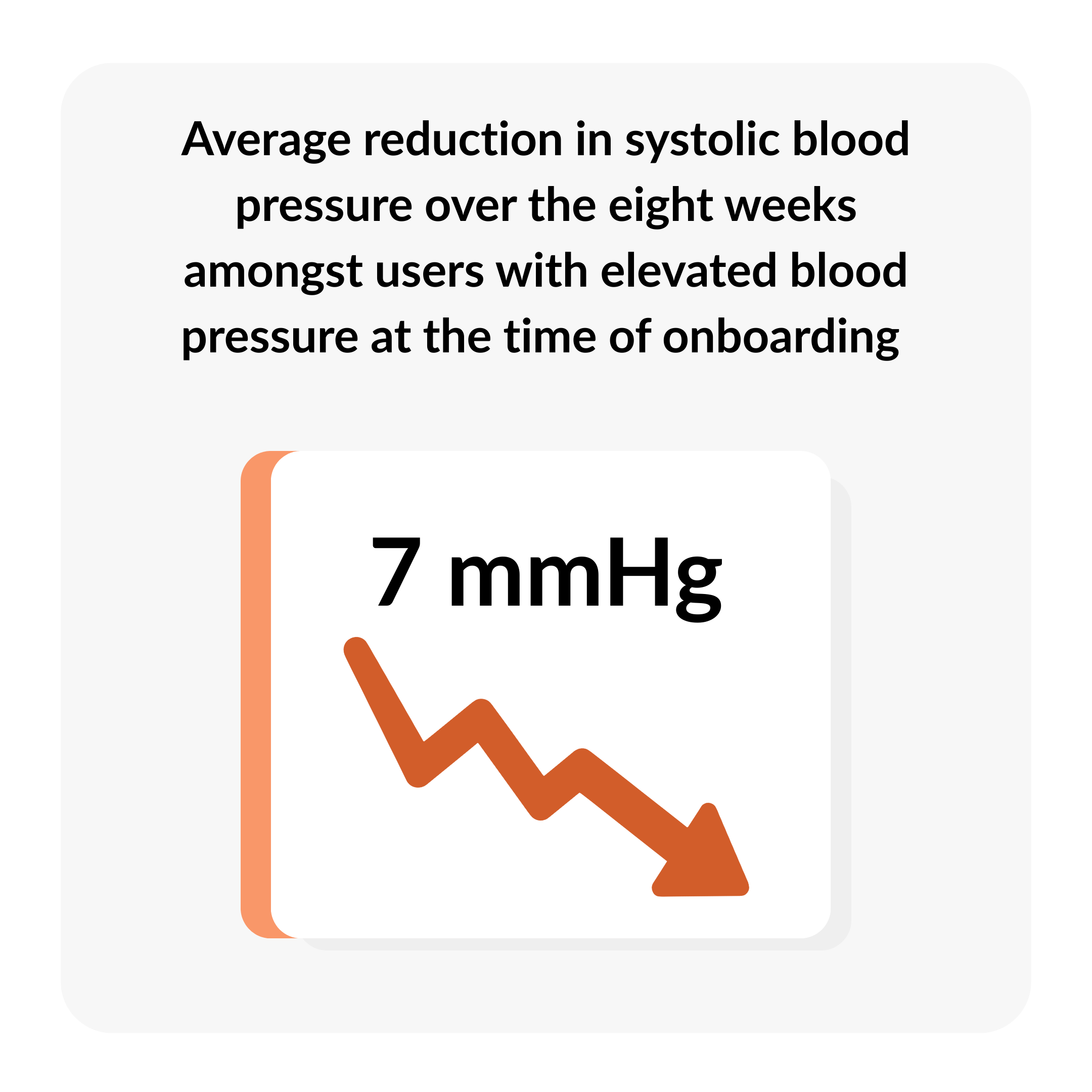
Measurable Improvements in Blood Pressure
For the core objective of this cohort, blood pressure management, the observed changes were encouraging. Among Holly Health users with elevated blood pressure at the time of onboarding (with a systolic BP reading of over 140), the average reduction in systolic blood pressure was 7 mmHg over the eight-week period. While further analysis would be required to assess statistical significance, the magnitude of this change is clinically relevant. Evidence from a large individual participant meta-analysis published in The Lancet indicates that a 5 mmHg reduction in systolic blood pressure is associated with an approximate 10% reduction in the risk of major cardiovascular events, including stroke (Rahimi et al., 2021).
Moving More Despite Barriers
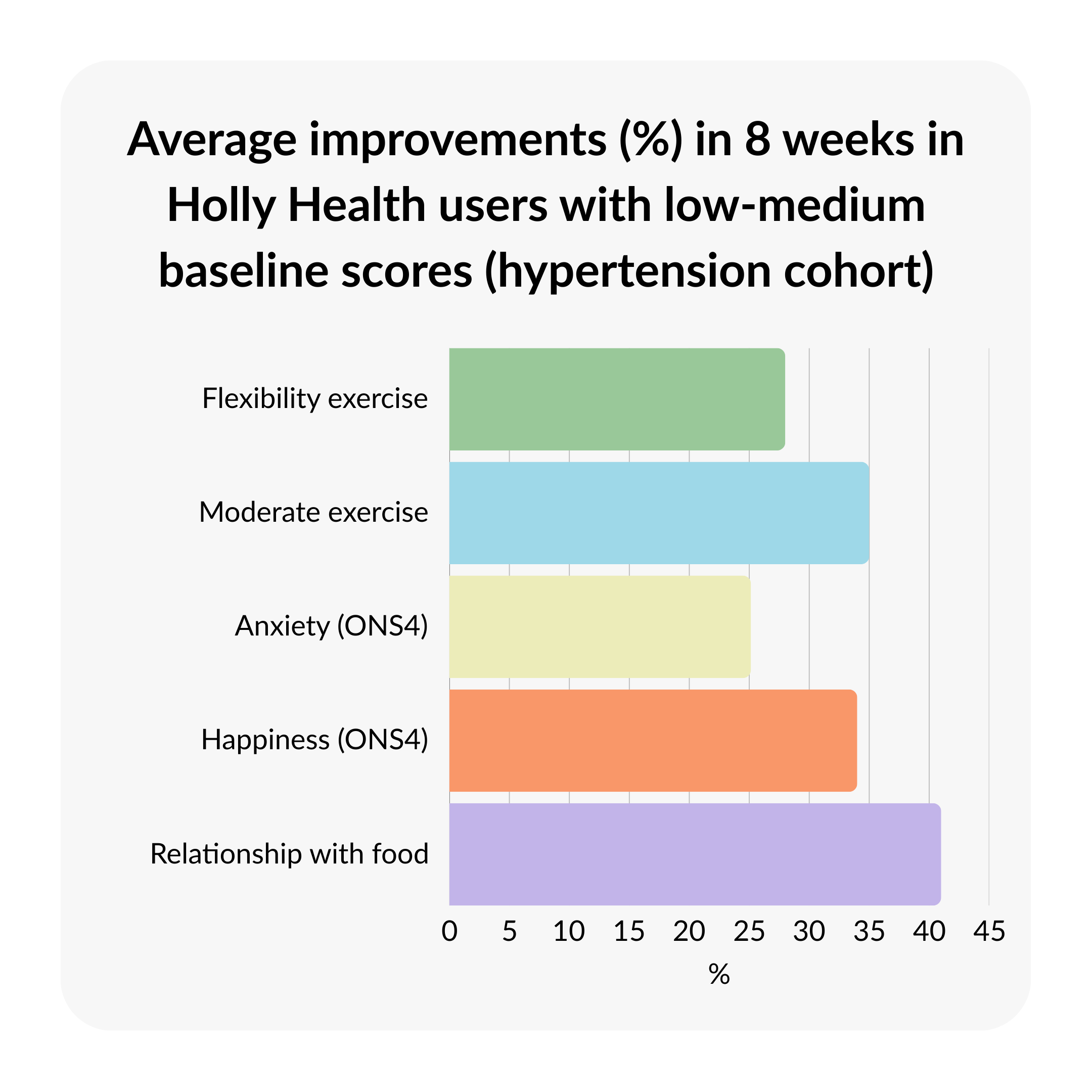
Despite the fatigue identified at baseline, users found ways to increase their physical activity levels. Moderate exercise scores increased by 35%, and flexibility exercise scores increased by 28%. Notably, users' data suggests this wasn't achieved through intensive gym routines, but through accessible habits. "Do some stretching" and "Do some walking" were among the most commonly adopted new habits. These simple, low-intensity movements appear to have provided a practical entry point for users to start building their activity levels.

Sustainable Weight Management
While many interventions focus on rapid weight loss, guidance from NICE emphasises the importance of sustainable, longer-term approaches to weight management (NICE, 2023). In this cohort, users achieved an average weight reduction of 3kg (approximately 3.3% of body weight). This was accompanied by a 14.5% increase in fruit and vegetable intake scores and a 41% reported improvement in their relationship with food. Together, these findings suggest a shift in eating patterns and behaviours, rather than short-term dietary restriction.
Mental Health Areas
The relationship between physical health and mental wellbeing was evident in the outcomes. Alongside physical changes, anxiety scores decreased by 25% (measured via ONS-4, where a lower score indicates improvement). Furthermore, scores for happiness increased by 34%. This suggests that supporting physical health management may have a protective or beneficial effect on mental wellbeing for this demographic, though the direction of causality cannot be established from this data.
Sustainability and Healthcare Impact
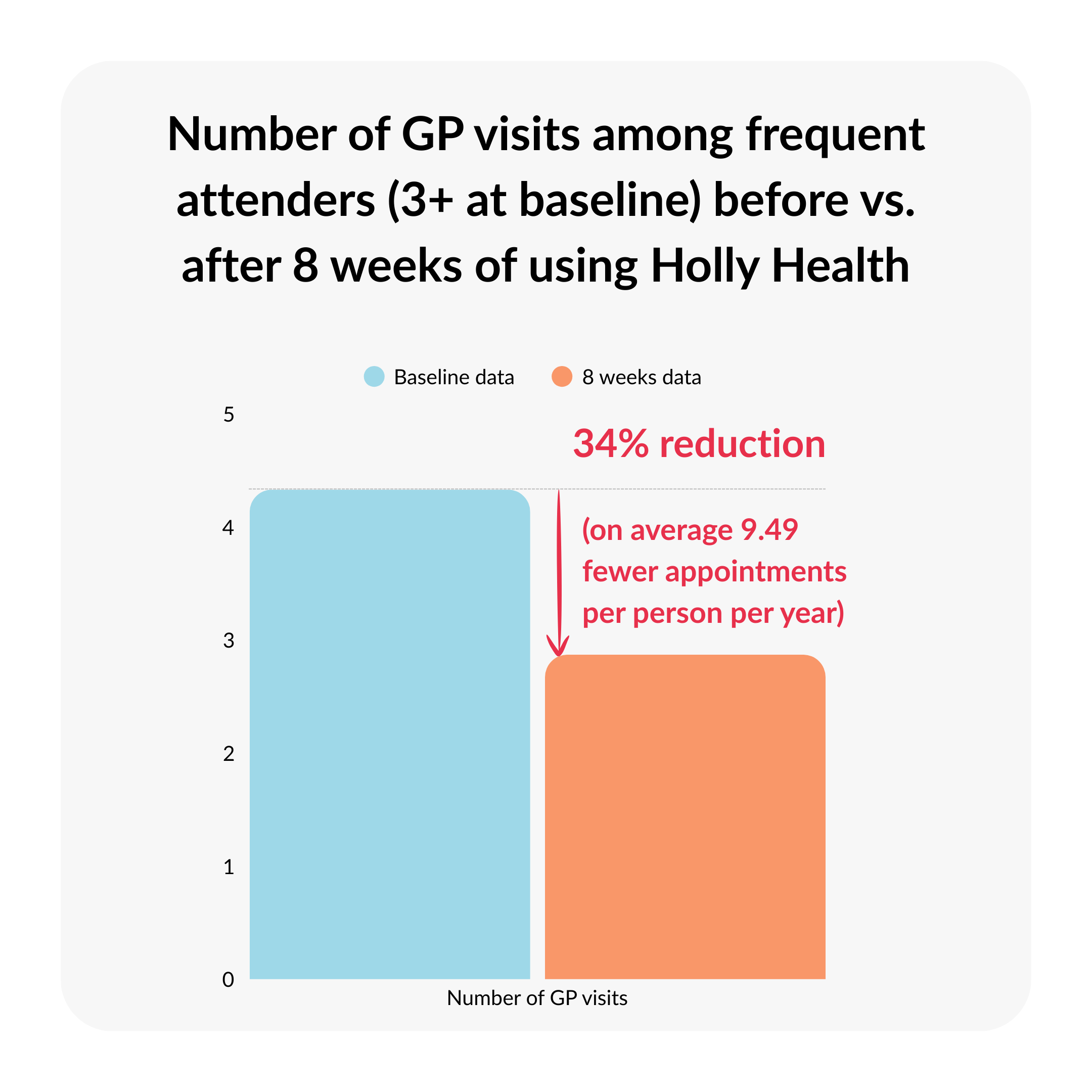
Perhaps the most critical metric for long-term success is sustainability. At the eight-week mark, 69% of users reported that they had developed one or more new health habits that they now do automatically. This shift from effortful behaviour change to automatic habit is particularly relevant for conditions like hypertension, which require lifelong management rather than short-term intervention.
Alongside these self-management improvements, a reduction in primary care usage was seen. Among ‘frequent attenders’ (those with three or more appointments at baseline), the data indicate 34% reduction in GP appointments, translating to 9.5 fewer appointments per high-service user per year. This reduction is notable for two reasons. First, it may reflect greater confidence and capability in managing day-to-day aspects of health, including blood pressure, physical activity and stress. Second, it highlights the potential for behaviour-change support to alleviate pressure on primary care services, particularly among individuals who typically have complex or ongoing health needs. While further research is needed to explore causality, these early indications suggest that helping people build sustainable health habits may enable them to manage more independently, reducing the need for repeated clinical appointments.
Conclusion
This analysis of 5,850 Holly Health users living with hypertension suggests that small, sustainable habit changes can translate into measurable health improvements. The observed 7mmHg average reduction in systolic blood pressure among users with elevated readings is encouraging, particularly when considered alongside the evidence linking blood pressure reduction to decreased cardiovascular risk (Rahimi et al., 2021). These changes occurred despite significant baseline barriers, including fatigue, poor sleep, and low activity levels; notably, these improvements were observed alongside adopting new accessible habits rather than intensive interventions.
The positive shifts observed across physical activity, dietary patterns and mental wellbeing highlight the interconnected nature of health behaviours. When individuals begin to make small, manageable adjustments - whether increasing movement, improving sleep, or reducing stress - the benefits often extend beyond the original focus area. In this cohort, these wider gains were accompanied by reports of improved energy, better mood and a more supportive relationship with food, suggesting that progress in one domain can help unlock progress in others.
Perhaps most importantly, 69% of users reported developing habits they now perform automatically, indicating these changes may be sustainable beyond the eight-week period. Whilst longer-term follow-up research would be beneficial to explore, these findings suggest that structured support for behaviour change may offer a practical approach to hypertension management for individuals who find traditional lifestyle advice difficult to implement. Taken together with the observed reduction in GP appointments among frequent attenders, these findings point to meaningful benefits not only for individuals, but also for the wider healthcare system, including reduced pressure on NHS primary care services.








.jpg)



